Tips from Child Psychologist, Emily Klass, on Putting the Phone Away at Night
Psst…For more helpful ways on managing screentime, check out Helpful Tools and Tips on How We Can Best Manage Kids’ Screen Time
Struggling to have your child to put down their phone and go to sleep at night? It was hard before the COVID-19 pandemic; now it just seems impossible. As a child psychologist, I hear story after story of children of all ages having extreme reactions to putting their phone away at night.
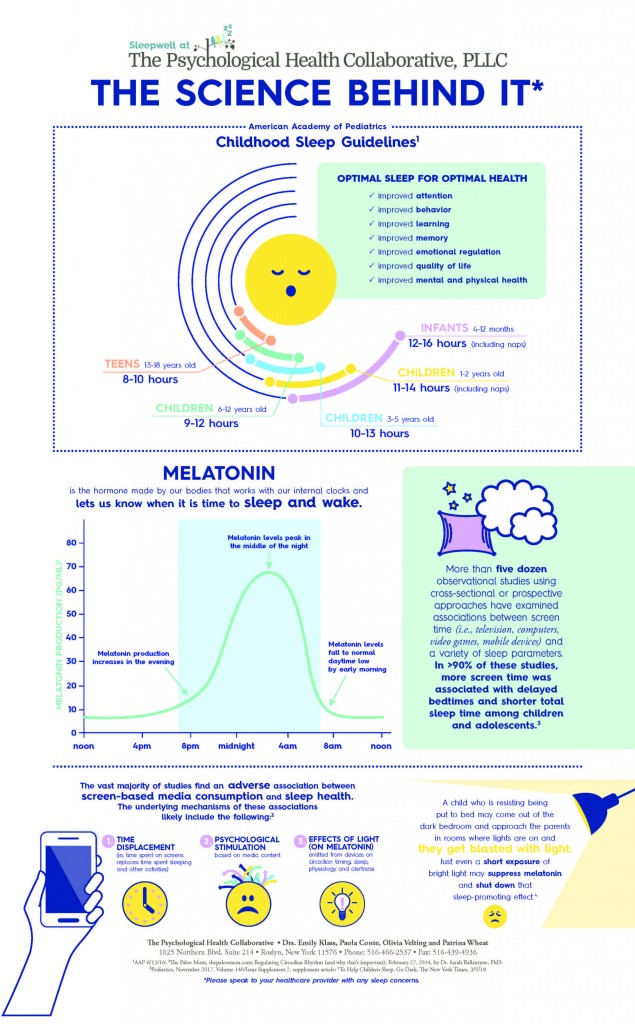
This extreme reaction interferes with the quality of sleep, sleep that is vital to healthy growth and development. Historically, we as parents have been deeply involved in the sleep of our infants and gradually move away from this close monitoring as they grow up, trusting that a reasonable bedtime and a bit of a routine will serve to allow the child to recharge their bodies and minds. This transition to sleep has been deeply disturbed by the presence of cell phones in the room, the bed, on the pillow of our kids. It is there during tiny mid-night awakenings and the light emanating is suppressing the hormone melatonin that provides for sleep.
The importance of sleep in child development is fact. Sleep deprivation damages children’s brains –normal plasticity – the adaptation of neural structures to the stimuli the brain receives is disrupted. The brain centers responsible for processing visual signals and sensory information are affected. Children are more apt to develop mood and anxiety problems. Those children who are more vulnerable, say with a diagnosis of ADHD, are even more highly affected. Worsened academic performance, obesity, poorer concentration is all evidenced.
In 2019, teens spent 7 hours and 22 minutes on the phone each day with tweens not far behind. Preschool-age children use smartphones and tablets longer than recommended and parents often don’t realize it. And those are preschoolers! When the phone is in the bedroom, children may not be able to separate from their phones and their usage is much longer than any of us know! How many parents have woken up in the middle of the night, expecting their children to be fast asleep, only to find out that their teen was on their phone most of the night? And children (and adults) steadfastly state the importance of what might happen if they are not!
Researchers, scientists, psychologists and parents know the hazards of too much smartphone use for our children. Sleep is critical to healthy child development. Sleep deprivation can alter the brain’s ability to adapt to change. Children who don’t get enough sleep are more likely to develop mood and anxiety problems. This is especially true of children with ADHD. A lack of sleep can also lead to problems with concentration, declining academic performance and obesity. The Mayo Clinic cautions that we must manage our children’s interface with smartphones.
Pre-pandemic, our children were deeply embedded in the electronic world. Since the pandemic, they have been forced to now even live their academic lives on their phones. And the phone has become an extension of their bodies. At the end of the arm and hand is the phone; ergonomically developed to fit perfectly and designed to maintain undivided attention with algorithmic coding.
Our children do best when their days follow reasonably predictable patterns and rhythms. Going off to school, changes and transitions during the school day, the return home, afternoon and evening activities and routines and bedtime. These normal markers of time help our children develop habits and routines that significantly help the development of healthy sleeping eating, mood regulation as well as the executive function skills – anticipation, planning, self-control, communication and self-confidence that are all reinforced with these structural scaffolds.
COVID has thrown all these time markers (across the whole 24 hours) in the air like a deck of cards. Not going into school at all, or going erratically, opening a laptop in bed — when the normal markers of time become ambiguous, our children have less opportunity to develop these routines and habits and skills. Establishing routines, habits — a healthy relationship with screens supports our children’s lives. The transition to sleep serves as a linchpin of this healthy relationship. Just emerging scientific research is compellingly telling us that our children are experiencing increasingly disrupted sleep schedules, sleep quality, extremely decreased opportunities for physical activity and way more sedentary behavior.
At night when we tell our kids to give us their phone, we might as well be telling them to cut off their hand – it is their friend, all they have learned during the day, pictures of their pets and their self-reflections, their fun, their social standing, their favorite book and song — their world.
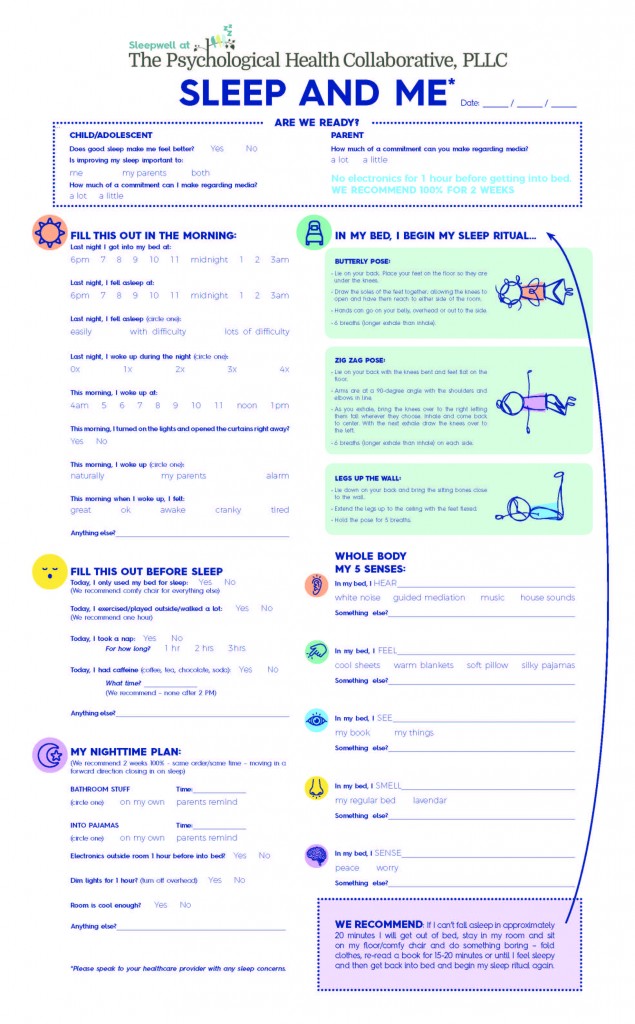
We can address the transition and quality of sleep in these proven ways:
1. The phone cannot be in the hand all day. The tie becomes too great, and separating too intense.
2. Keep a bedtime ritual – from super simple to elaborate. Use a ritual that works for your child and your family. Perhaps it is a quick teeth brush and then jump into bed or perhaps all animals real to stuffed and parents must be kissed, lights checked, etc. When there is a bit of a ritual, separating from the phone can be incorporated into it.
3. Mirror your expectation of them in your own behavior: children are quick to indict parents for being glued to screens.
4. Put the phone to bed. Let it recharge while we all recharge.
In my office I have long had a little doll’s bed – children, teens, and even adults “tuck” their phones in, freeing themselves to concentrate on our sessions.
With my industrial design partner, I have invented a product called KozyFone for us all, to tuck in and recharge our phones while we and our children are recharging. It offers a new part of our bedtime rituals – marked by this tucking-in – to promote better sleep hygiene to children in a positive way. It is part of the sleep ritual (and recharges the phone) and I wrote a manual for helping our children to go off to sleep incorporating the evidence-based information we now have.
To support our mission of improving children’s sleep health and relationship with technology, you can learn more about our product here: KozyFone-Kickstarter-Panels.pdf